
Perforated patch clamp: from pores to currents and the challenges in between

by Clara Lenherr, PhD student, Burrone Lab, MRC Centre for Neurodevelopmental Disorders, King's College London
The problem with whole-cell patch clamp
Patch clamping is a common electrophysiological technique used to study the electrical behaviour of single neurons in the brain. The most commonly used variety of patch clamp is the whole-cell method, which involves forming a tight high-resistance seal onto the membrane of a cell and subsequently breaking the membrane with force to achieve a continuum between the patch pipette and the cell’s cytosolic solution, allowing for full electrical access. Whole-cell mode is useful for recording voltage or current responses from cells with a very low access resistance.
However, whole-cell patch clamp inevitably involves artificially manipulating the cell’s cytosolic composition as it mixes with the solution in the pipette. Pipettes are therefore normally filled with an “intracellular” solution that mimics the ionic composition inside the neurons they are targeting. However, the intracellular solution is a simplified version of the cell’s cytosolic contents, and mainly mimics the concentrations of the major ions that determine the resting membrane potential (sodium, potassium, and chloride). This often results in washout of key endogenous cytosolic signalling molecules, such as cAMP and ATPase, which could disrupt receptor-mediated downstream signalling pathways. Normal intracellular calcium buffering is also affected, as exogenous calcium buffers such as EGTA are normally added to the pipette solution. These cytosolic components that are prone to washout are especially crucial in synaptic plasticity events, which are among the most commonly studied using patch clamp. Thus, there is a need for a method that enables electrophysiological recordings without altering the cell’s cytosolic composition, but still achieves a relatively low access resistance.

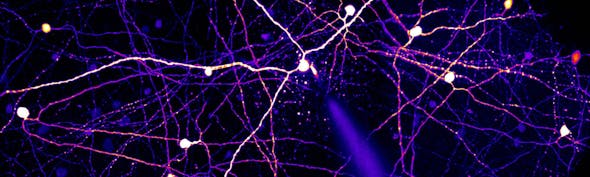
Patch clamp techniques (from L to R) - Cell-attached, Whole Cell and Perforated Patch
A less invasive patch clamp technique
In 1988, Horn & Marty1 first reported a variation of the patch clamp technique, termed perforated patch, which involves applying pore-forming agents to the pipette solution to perforate, rather than rupture, the membrane patch. The equilibration between the pipette and cytosolic solution is determined by the permeability properties of the pore-forming agent, normally an antibiotic. Two commonly used antibiotics are nystatin and amphotericin B, which both make the membrane permeable to small monovalent cations and anions (sodium, potassium, chloride), but impermeable to divalent or large ions, including calcium and intracellular signalling molecules2. This has been extremely useful for determining properties of calcium currents, including those mediated by NMDA receptors, without modulating intracellular calcium concentrations. These techniques have been particularly useful for studying synaptic plasticity mechanisms.
Gramicidin perforated patch: The dance between chloride and GABA
The perforated patch technique has also played a major role in shaping our understanding of the major inhibitory neurotransmitter in the brain, GABA. GABAergic neurotransmission has proven to be much more complex than we first thought, particularly during development, as it can have both depolarising and hyperpolarising effects. GABA receptors themselves are chloride channels, meaning that the concentration of chloride in neurons is the main determinant of the polarity (depolarising or hyperpolarising) of GABA-mediated currents. By using another pore-forming antibiotic, gramicidin, that forms pores which are permeable to small monovalent ions (sodium, potassium) but not anions like chloride, GABA-mediated currents can be measured without interfering with the intracellular chloride concentration3,4.
Based largely on gramicidin perforated patch recordings, it was shown that the chloride reversal potential, the membrane potential at which the net flow of chloride ions across the membrane is zero, gradually decreases across development, indicating a gradual decrease in intracellular chloride concentration5. This led to the fundamental discovery that GABA switches from depolarising early in development to hyperpolarising in adults6. The development of this technique has therefore been particularly crucial in advancing our understanding of GABAergic neurotransmission across life.
The challenges of gramicidin perforated patch
Despite its clear advantages, perforated patch comes with several technical challenges, which I discovered myself when attempting the technique. Firstly, you have to achieve a very stable gigaseal with the membrane for successful perforation to occur. Gramicidin perforation is particularly slow, normally taking around 20 minutes to perforate, making it more technically challenging to work with than other perforants. Antibiotics at the tip of the pipette can also affect gigaseal formation, and may begin to degrade cellular membranes if leaked onto the slice. For this reason, it is preferable to front-fill the pipette with solution that does not contain any drug, then back-fill with the drug-containing solution, and apply a smaller positive pressure than usual. Seal formation should then be achieved as rapidly as possible, before the antibiotic diffuses to the tip.
The membrane integrity of cells, particularly at the membrane patch, is key for a successful perforation. Several experimental parameters must therefore be optimised, including the concentration of the antibiotic, the osmolarity of the pipette solution, and the size and shape of the pipette tip. The concentration of the antibiotic can vary greatly depending on which one is used. Gramicidin is normally used at 20-50µg/mL whereas lower concentrations of nystatin (2-4 µg/mL) and amphotericin B (0.1-0.2 µg/mL) are required. The temperature of the perfusion bath and, if using ex vivo brain slices, the age of the animal and slicing method will also influence membrane integrity, and ease of both seal formation and perforation.
Attention should be given to how the antibiotic-containing pipette solution is prepared, since this can affect the structural conformation of gramicidin which influences its pore-forming abilities. In the literature, there is very limited information about the solvents and methods used for gramicidin perforation, but it is commonly dissolved in DMSO or methanol and heated and/or sonicated to dissolve.
Most importantly, spontaneous rupture of the membrane must be avoided. The extent of perforation is normally monitored by continuously applying a test voltage step and recording the capacitive current, to gauge the access resistance between the pipette and the membrane. A successful perforation will be indicated by a gradual decrease in access resistance to a minimum value of ~10-20MΩ for all three perforation agents7. To ensure that a drop in access resistance is the result of true perforation and not spontaneous rupture, it is necessary to add a membrane-impermeable dye to the pipette solution so that you can visualise whether the dye enters and fills the neuron you are recording from- a filled neuron means that you have ruptured the membrane and entered whole-cell mode. Alternatively, you can add a sodium channel blocker to the pipette solution and test whether the neuron is able to fire- if spontaneous rupture occurs then the sodium channel blocker will enter the cell and prevent firing.
Overall, gramicidin perforated patch is a useful but challenging technique to master. It is therefore not surprising that it is much less commonly used compared to nystatin or amphotericin B. When carrying out perforated patch, it is extremely important to validate that perforation, rather than spontaneous rupture, is occurring. Nonetheless, the advantages of all forms of perforated patch are very clear, with each one allowing researchers to address distinct sets of questions.
References
About Clara
Clara is a PhD student in Professor Juan Burrone’s lab at the MRC Centre for Neurodevelopmental Disorders at King's College London, where she is researching activity-dependent plasticity of inhibitory neurons.
She is also the co-host of the Neuroverse Podcast series.




)