The top neuroscience research from March 2021
Discovery of ‘zombie cells’ that increase their activity following death, proven effectiveness of a mutation-specific vaccine against brain tumours, and a skin test for detecting Parkinson’s disease are included in this month’s top neuroscience research news. We hope you find these as interesting as we do!
1. Researchers discover new potential for functional recovery after spinal cord injury
A type of glial cell in the central nervous system has been successfully reprogrammed by scientists at Indiana University School of Medicine to become new neurons, promoting recovery following spinal cord injury.
This is the first time that NG2 glial cells have been modified to become functional neurons following spinal cord injury. The researchers achieved this by increasing levels of the SOX2 transcription factor, enabling glia-to-neuron conversion at the site of injury, with reduced glial scar formation and increased functional recovery.
This type of glial cell is now an important target for the development of treatments for spinal cord injury.
Potential new treatment for spinal cord injury
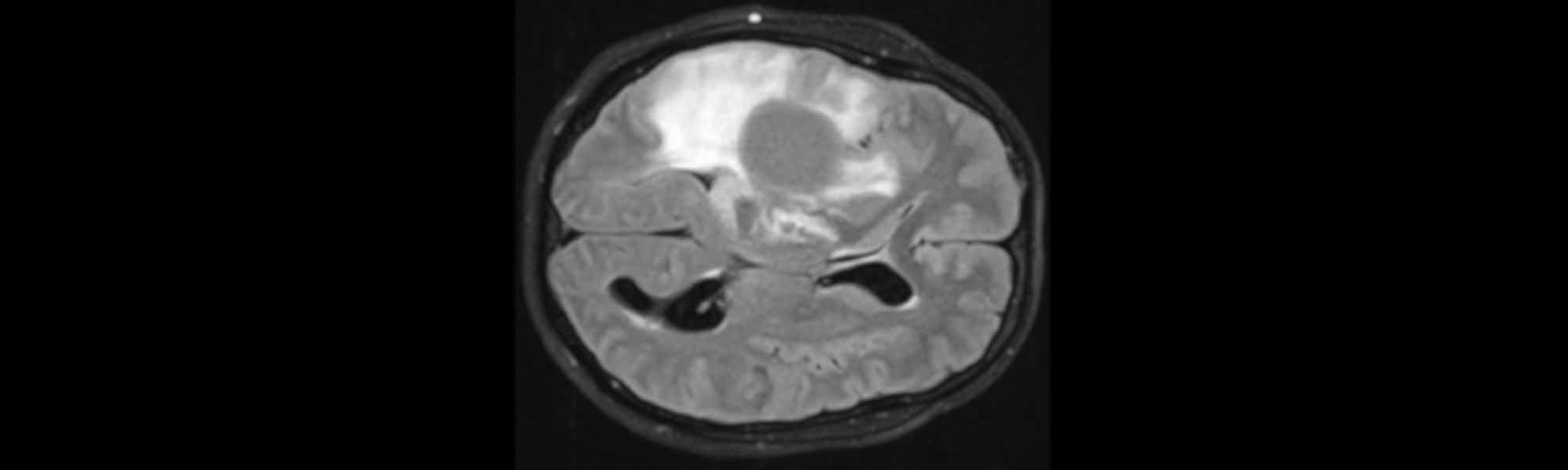
2. Vaccination against mutated protein tested in brain tumour patients for the first time
A mutation-specific vaccine against malignant brain tumours has been found by researchers at the German Cancer Research Center, University Medicine Mannheim, Heidelberg University Hospital, and the National Center for Tumor Diseases (NCT) Heidelberg to safely and effectively activate the desired immune response in tumour tissue.
The vaccine targets diffuse gliomas, which are usually incurable brain tumours that are difficult to complete remove using surgery, with chemotherapy and radiotherapy only having a limited effect. The tumour cells have the same gene mutation in over 70% of patients, which creates a novel protein structure in the IDH1 enzyme. This neo-epitope can be recognised as foreign by the patient’s immune system.
The aim of the vaccine is to alert the patient’s immune system to the presence of the neo-epitope. As this mutation is only present in the glioma cells, and is what causes glioma development, targeting it is tackling the root of the problem.
Out of 33 patients who received the vaccine, an immune response was able to be evaluated in 30. 93% of these patients showed a specific immune response to the vaccine peptide, and a large proportion of patients showed 'pseudoprogression', which is swelling of the tumour caused by a host of invading immune cells. In fully vaccinated patients, the three year survival rate following treatment was 84%.
A phase II study is now being planned, with the hope that this treatment could effectively halt tumour progression.

Promising vaccine for deadly brain tumours
3. Research shows some genes come to life in the brain after death
A new study from the University of Illinois Chicago discovered that in the hours after we die, some cells in the human brain remain active. Certain cells even increase their activity and show large growth.
The researchers analysed gene expression in brain tissue, collected during routine brain surgery, multiple times following removal to simulate the post-mortem interval and death. They discovered that some cells have increased gene expression after death.
Genes that increased expression following the post-mortem interval, termed ‘zombie genes’, were specific to glial cells only. It was found that glial cells grow and develop arm-like appendages for hours following death.
This finding is important, as it means that these genetic and cellular changes need to be accounted for in studies that use post-mortem human brain tissue, which is often used to research treatments for disorders such as autism, schizophrenia and Alzheimer’s disease.

Important finding for neuroscience research
4. Study links genes with function across the human brain
A map that links gene signatures to functional processes across the human brain has been produced by scientists at McGill University. This provides insight into how human thoughts and emotions arise from specific genes, pathways and cell types.
The map was generated from machine learning analysis of the gene expression atlas from the Allen Human Brain Atlas and the functional association map from Nerosynth. This revealed links between gene expression patterns and functional brain tasks such as memory, attention, and mood.
A clear genetic signal that separates cognitive processes, such as attention, from affective processes, like fear, was discovered. The researchers were able to trace this separation to gene expression in specific types of cells and molecular pathways, which could prove useful for future research into psychiatric disorders. Identifying these molecular signatures for different psychological processes will enable greater understanding of how human thoughts and emotions arise, and could provide new targets for future treatments.
Find out more
5. Time needed to sequence key molecules could be reduced from years to minutes
A potentially new way to sequence glycosaminoglycans, a class of long chain-linked sugar molecules, which could reduce the time taken from years to minutes, has been developed by scientists at Rensselaer Polytechnic Institute.
Glycosaminoglycans (GAGs) are found on cell surfaces and extracellular matrices of all animals, and are involved in cell growth, cell signalling, anticoagulation and wound repair. Similarly to DNA, GAGs can be subdivided into the disaccharide sugar units that they are composed of. However, DNA is made of four letters in a linear string, whereas GAGs have dozens of basic units, some of which have sulfate, acid and amide groups attached. This makes glycan sequencing difficult and time-consuming, involving sophisticated analysis.
Using a nanopore device and state of the art machine learning tools, the researchers have demonstrated that GAGs could be sequenced in real-time, saving years of effort. This proof of concept will be further developed to teach the device to read more complex GAGs.

Simplifying a complex process
6. Scientists move closer to developing ‘game-changing’ test to diagnose Parkinson’s
Scientists at the University of Manchester have developed a technique that analyses compounds found on the surface of the skin to detect Parkinson’s disease.
The test works by analysing compounds found in sebum, which is an oily substance that coats the skin to protect it. It is thought that people with Parkinson’s may produce more sebum than normal, which is a condition called seborrhoea.
In this study, high resolution mass spectrometry was used to profile the chemical signature of sebum in people with Parkinson’s disease. It was found that the chemical signature changes as the condition progresses, including changes in lipid processing and mitochondria.
This quick and simple method of testing could not only diagnose Parkinson’s disease but monitor the development of the condition. The test could be used to help test new treatments and see if they are successful at stopping or slowing down disease progression.

Better detection and monitoring of Parkinson's disease
7. Focusing on the unhealthy brain to speed drug discovery
A collaboration of researchers from the University of Houston and National Institutes of Health has led to the development of a new open-source toolkit that speeds up the discovery of drugs to treat a range of brain diseases and injuries.
The researchers developed an innovative imaging technique that combines high-resolution images of whole brain slices with a computational image analysis method based on deep neural networks. By using these methods to map and profile unhealthy and drug-treated brain tissue in unprecedented detail, multiple biological processes can be shown at the same time. For example, a brain injury, effects of a drug on the brain injury and the potential side effects of the drug.
This is a more flexible, scalable and efficient way to screen drugs, enabling more rapid drug development.

Speeding up drug discovery
8. New test enables rapid detection of mild cognitive impairment as well as dementia
A new computerised cognitive test that enables rapid detection of mild cognitive impairment and dementia has been developed by researchers at Kanazawa University.
The test, termed computerised assessment battery for cognition (C-ABC), effectively screens for both dementia and mild cognitive impairment (MCI) in just five minutes, compared to existing tests taking 10-30 minutes to complete. Existing tests don’t screen for both dementia and MCI, whereas this new test can accurately screen for both conditions.
This tool could make cognitive screening more accessible as well as more accurate and efficient, enabling dementia and MCI to be detected earlier. This in turn could improve treatment options and outcomes for patients with these conditions.

Computerised test for improved cognitive screening
9. Experimental hearing implant succeeds in registering brain waves
Researchers at KU Leuven have successfully used a cochlear implant to measure brain waves for the first time.
These brain waves can be used to measure hearing quality, and are therefore a step towards development of smart hearing aids, where a cochlear implant automatically adjusts based on how a person processes the sounds they hear. This would enable a person’s hearing to be monitored in everyday life, reducing the need for regular testing at hospitals, and improving the quality of life of patients.

Read more
10. New brain sensor offers Alzheimer’s answers
A tool to monitor how brain cells communicate has been developed for the first time by researchers at UVA.
By examining this communication in healthy and diseased brains, huge improvements could be made to scientists’ understanding of and treatment developments for depression, sleep disorders autism and other neurological and psychiatric conditions.
Monitoring brain cell communication for the first time
Banner image credit: © Universitätsmedizin Mannheim

)